The Risk of Ovarian Cancer After Total Hysterectomy
In modern medicine, hysterectomy is a common surgical procedure that involves the removal of a woman's uterus. Significant for various medical reasons, from chronic pelvic pain to uterine fibroids, total hysterectomy may also involve the removal of the cervix, ovaries, and fallopian tubes. However, a question lingering among many women is the risk of ovarian cancer after total hysterectomy. This article delves into the implications, risks, and considerations surrounding this essential topic to provide a comprehensive understanding.
Understanding Hysterectomy: Definitions and Types
A hysterectomy can be categorized into different types based on the surgical approach and extent of the operation:
- Total Hysterectomy: This involves the removal of the uterus and cervix.
- Subtotal (or Partial) Hysterectomy: In this procedure, only the uterus is removed, leaving the cervix intact.
- Radical Hysterectomy: This includes the removal of the uterus, cervix, surrounding tissue, and possibly some part of the vaginal canal.
- Salpingo-Oophorectomy: Often performed alongside a hysterectomy, this involves the removal of the ovaries and fallopian tubes.
The Importance of Ovarian Health
The ovaries play a crucial role in the female reproductive system by producing hormones such as estrogen and progesterone. These hormones are essential not only for reproductive health but also for overall health in women. With the removal of the ovaries, hormonal balance may be disrupted, leading to a variety of health consequences.
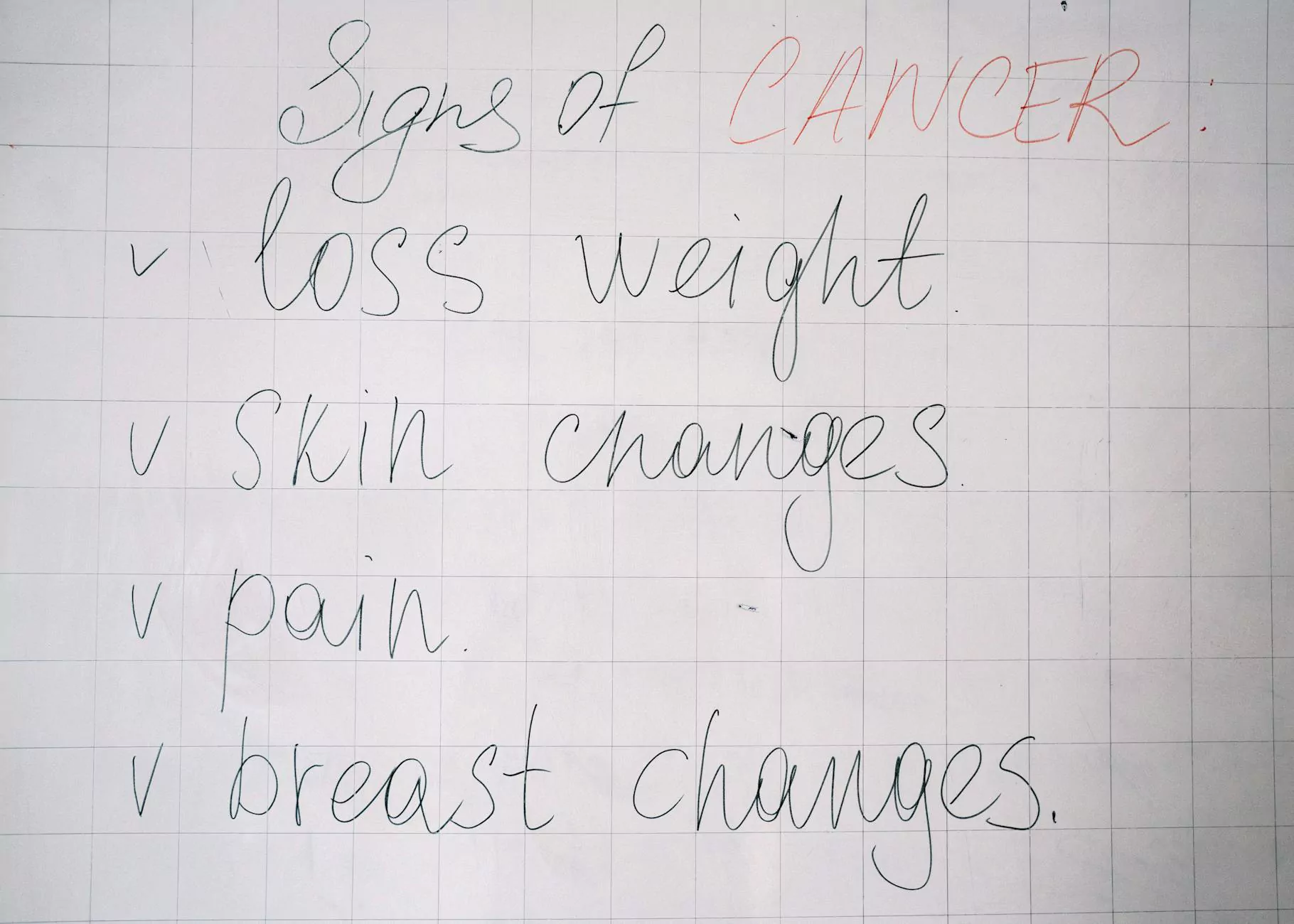
Ovarian Cancer: An Overview
Ovarian cancer is a malignant tumor that begins in the ovaries. It can go undetected until it has reached advanced stages due to subtle early symptoms. Statistics show that ovarian cancer accounts for a significant number of cancer-related deaths among women. Understanding the factors that contribute to its risk is vital for prevention and management.
Risk Factors for Ovarian Cancer
Several factors can increase the risk of ovarian cancer:
- Genetic Predisposition: Women with mutations in the BRCA1 or BRCA2 genes have a higher risk of developing ovarian cancer.
- Family History: A family history of ovarian or breast cancer can elevate personal risk.
- Age: The risk of ovarian cancer increases as women age, particularly after menopause.
- Personal Medical History: Women with a history of endometriosis or previous cancers may be at greater risk.
- Reproductive Factors: Factors like never having been pregnant or having irregular menstrual cycles can impact risk.
Does Total Hysterectomy Increase the Risk of Ovarian Cancer?
The question arises: Does undergoing a total hysterectomy increase the risk of ovarian cancer after total hysterectomy? This is a multifaceted issue, as it largely depends on whether the ovaries are removed during the hysterectomy and individual health circumstances.
The Ovaries and Hysterectomy
If a total hysterectomy includes the removal of the ovaries (a procedure known as bilateral salpingo-oophorectomy), this significantly reduces the risk of ovarian cancer, as the primary source of such cancers is no longer present. However, if the ovaries are retained, the risk still persists.
Impact of Hormonal Changes
After a hysterectomy, especially if the ovaries are removed, women may experience a rapid decrease in hormone levels. This can lead to surgical menopause, with symptoms including:
- Hot flashes
- Night sweats
- Vaginal dryness
- Emotional changes
This sudden change in hormone levels can also have implications for long-term health, including cardiovascular health, bone density, and even potential risks related to other cancers.
Statistical Insights into Ovarian Cancer Risk
Research indicates that women who have undergone a total hysterectomy with ovary removal have a significantly lower incidence of ovarian cancer. In contrast, those who keep their ovaries post-hysterectomy may have a risk comparable to women in the general population. According to studies, the lifetime risk of ovarian cancer for women in the general population is about 1.3%, but this drops drastically for those who have had their ovaries removed.
Monitoring and Screening Post-Hysterectomy
For women who have kept their ovaries, ongoing monitoring and routine gynecological exams remain crucial. Regular screenings, including pelvic examinations and ultrasounds when appropriate, allow for early detection of potential cancers or abnormalities. It is recommended that women maintain a dialogue with their healthcare providers about risk factors and recommended screening methods.
The Role of Genetics in Risk Assessment
Given the significant hereditary component in many cases of ovarian cancer, genetic counseling may be warranted for women with substantial family histories of gynecologic cancers. Testing for genetic mutations can guide decision-making regarding prophylactic surgeries or enhanced surveillance.
Health Tips for Women Post-Hysterectomy
Maintaining optimal health after a total hysterectomy involves various strategies, including:
- Regular Check-ups: Ensure you attend all scheduled medical appointments.
- Healthy Diet: Incorporate a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health.
- Physical Activity: Engage in regular exercise to help maintain healthy body weight and reduce cancer risk.
- Listen to Your Body: Be mindful of any changes or symptoms and report them to your physician promptly.
- Mental Health: Seek resources for counseling or support groups if needed, to deal with emotional changes.
Consulting Healthcare Providers
The importance of collaborative care cannot be overstated. Patients should work closely with a team of healthcare providers, including:
- Gynecologists: For routine examinations and issues specific to female reproductive health.
- Primary Care Physicians: For overall health monitoring after surgery.
- Oncologists: If there are elevated concerns about cancer risks.
Conclusion: Empowering Women Through Knowledge
Understanding the risk of ovarian cancer after total hysterectomy is essential for informed decision-making and proactive health management. Through comprehensive discussions with healthcare professionals, awareness of personal and familial risk factors, and healthy lifestyle choices, women can navigate life post-hysterectomy with confidence. Knowledge is power, and empowering women with accurate information can significantly influence their overall health trajectories.
For more insights and detailed guidance on this topic, visit drseckin.com, where women can find a wealth of resources dedicated to gynecological health and wellness.