Understanding the Full Hysterectomy Risks

Introduction to Full Hysterectomy
A full hysterectomy is a surgical procedure involving the removal of the entire uterus and, in some cases, surrounding structures such as the cervix, fallopian tubes, and ovaries. This procedure is generally recommended for various medical reasons, including chronic pain, heavy bleeding, fibroids, and cancer. While it can significantly improve the quality of life for many patients, it is crucial to understand the associated risks. In this article, we will delve into the full hysterectomy risks, the benefits of the procedure, and how to navigate the decision-making process.
Common Reasons for a Full Hysterectomy
Full hysterectomies might be performed for several reasons, including but not limited to:
- Uterine Fibroids: Noncancerous growths that can cause pain and heavy bleeding.
- Endometriosis: A painful condition where tissue similar to the lining inside the uterus grows outside it.
- Cancer: Uterine, cervical, or ovarian cancers may necessitate removal to prevent the spread of disease.
- Chronic Pelvic Pain: Persistent pain can lead to a reduced quality of life and may require surgical intervention.
Understanding these reasons can help patients make more informed choices about their reproductive health options.
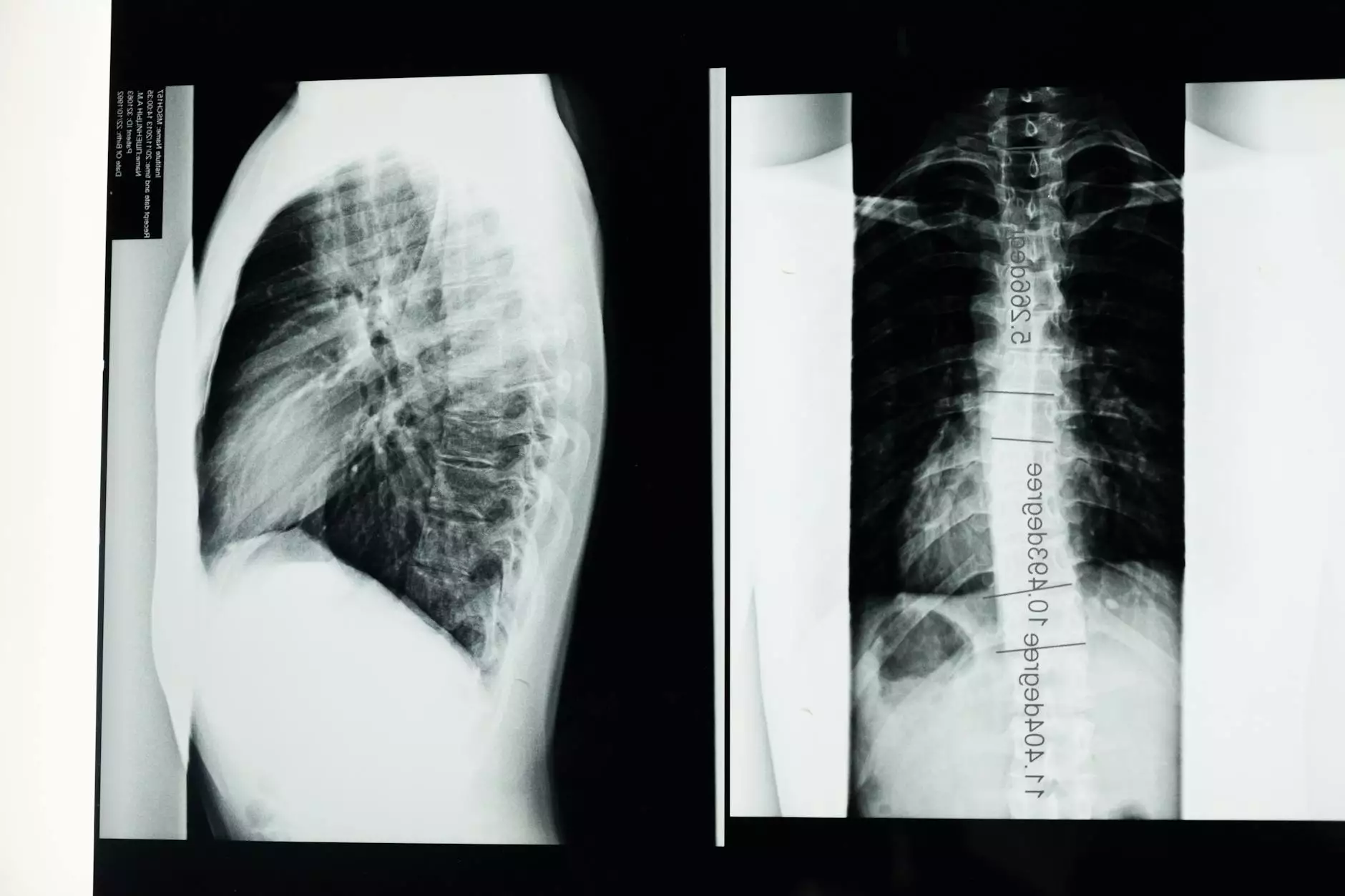
Types of Hysterectomy Procedures
There are generally three types of hysterectomy procedures:
- Total Hysterectomy: Removal of the uterus and cervix.
- Subtotal (or Partial) Hysterectomy: Removal of the uterus, leaving the cervix intact.
- Radical Hysterectomy: Removal of the uterus, cervix, surrounding tissues, and possibly parts of the vagina and nearby lymph nodes. This is typically done when cancer is involved.
Each type has its specific implications and risks, which should be thoroughly discussed with a healthcare provider.
Full Hysterectomy Risks
Like any major surgery, a full hysterectomy carries its own set of risks. Understanding these can empower patients to make informed decisions regarding their health:
Short-term Risks
Immediately following the surgery, patients may encounter some common risks, including:
- Infection: Surgical sites can become infected, leading to fever and other complications.
- Blood Clots: The risk of blood clots in the legs or lungs increases after surgery.
- Bleeding: Excessive bleeding during or after the procedure may require further medical intervention.
- Anesthesia Risks: Reactions to anesthesia, while rare, can occur and may lead to complications.
Long-term Risks
Long-term risks are essential to consider as well, including:
- Hormonal Changes: If the ovaries are removed, patients may experience menopause symptoms such as hot flashes and mood swings.
- Sexual Dysfunction: Changes in sexual function, including decreased libido or painful intercourse, can occur due to the removal of ovaries and changes in anatomy.
- Emotional Impact: Feelings of anxiety and depression may arise due to hormonal fluctuations or the psychological effects of losing reproductive organs.
- Prolapse: Other pelvic organs may weaken and lead to issues such as bladder or bowel dysfunction.
It’s crucial for patients to discuss these risks openly with their healthcare provider to fully understand the implications of undergoing a full hysterectomy.
Benefits of a Full Hysterectomy
Despite the risks, a full hysterectomy can provide numerous benefits, improving the quality of life for many women, such as:
- Relief from Symptoms: Immediate alleviation from chronic pain, heavy bleeding, and other distressing symptoms.
- Reduced Cancer Risk: Removal of cancerous tissues can prevent the spread of malignant cells and improve survival rates.
- Improved Quality of Life: Many women experience a significant increase in their daily quality of life post-surgery when debilitating symptoms are resolved.
Making an Informed Decision
Making the choice to undergo a full hysterectomy requires careful consideration of the risks and benefits. Here are some steps to help you make an informed decision:
- Consult with a Specialist: Seek advice from a qualified obstetrician-gynecologist to discuss your specific situation.
- Get a Second Opinion: If uncertain, consult another expert to confirm the necessity of the procedure.
- Consider All Treatment Options: Explore alternative treatments that may be available for your condition before committing to surgery.
- Discuss Concerns: Openly communicate your fears and hopes about the surgery with your healthcare provider.
Being proactive in your healthcare can significantly influence your experience and outcomes.
Post-Operative Care and Recovery
Post-operative care is critical for a successful recovery after a full hysterectomy. Consider the following:
Initially After Surgery
In the first few weeks following the surgery, patients should:
- Rest: Limit physical activity and allow your body time to heal.
- Manage Pain: Use prescribed medications to manage discomfort effectively.
- Monitor for Complications: Watch for signs of infection or unusual symptoms and contact your doctor if concerns arise.
Long-term Health and Wellness
For long-term health, consider integrating the following habits:
- Regular Check-ups: Schedule regular visits with your healthcare provider to monitor your overall health.
- Healthy Lifestyle: Adopt a balanced diet and engage in regular physical activity to maintain physical and mental well-being.
- Seek Support: Consider joining support groups or therapy to navigate emotional changes post-surgery.
Conclusion
In summary, a full hysterectomy is a significant surgical procedure with its unique set of risks and benefits. Understanding the implications of undergoing this surgery is essential for patients. By collaborating closely with healthcare professionals and making informed choices, women can navigate their health journeys more effectively. Ultimately, the goal is to achieve a healthier, more fulfilling life. For more information about full hysterectomies and personalized health advice, visit Dr. Seckin's website.